















At the University of Washington, virologist Angela Rasmussen has made game-changing advances in modeling Ebola virus with mice. Along the way, she used CLC Genomics Workbench and Ingenuity® Pathway Analysis to discover important details about host genetics and infection.

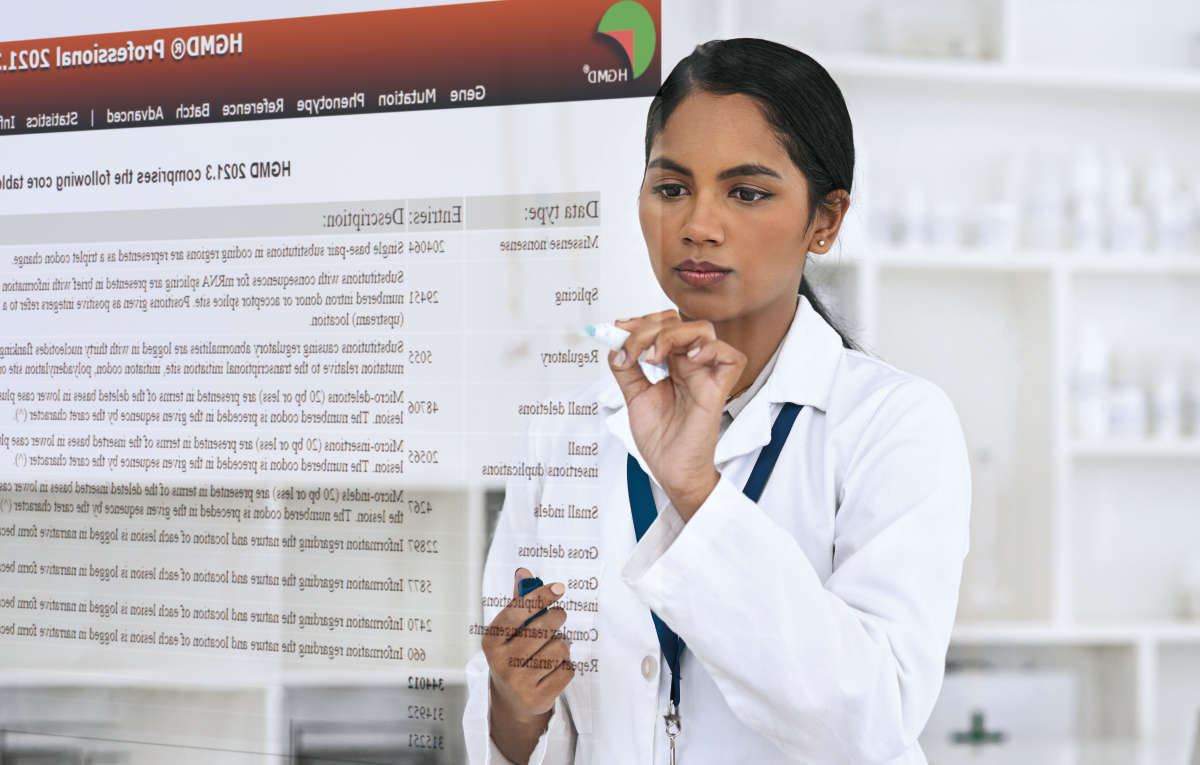
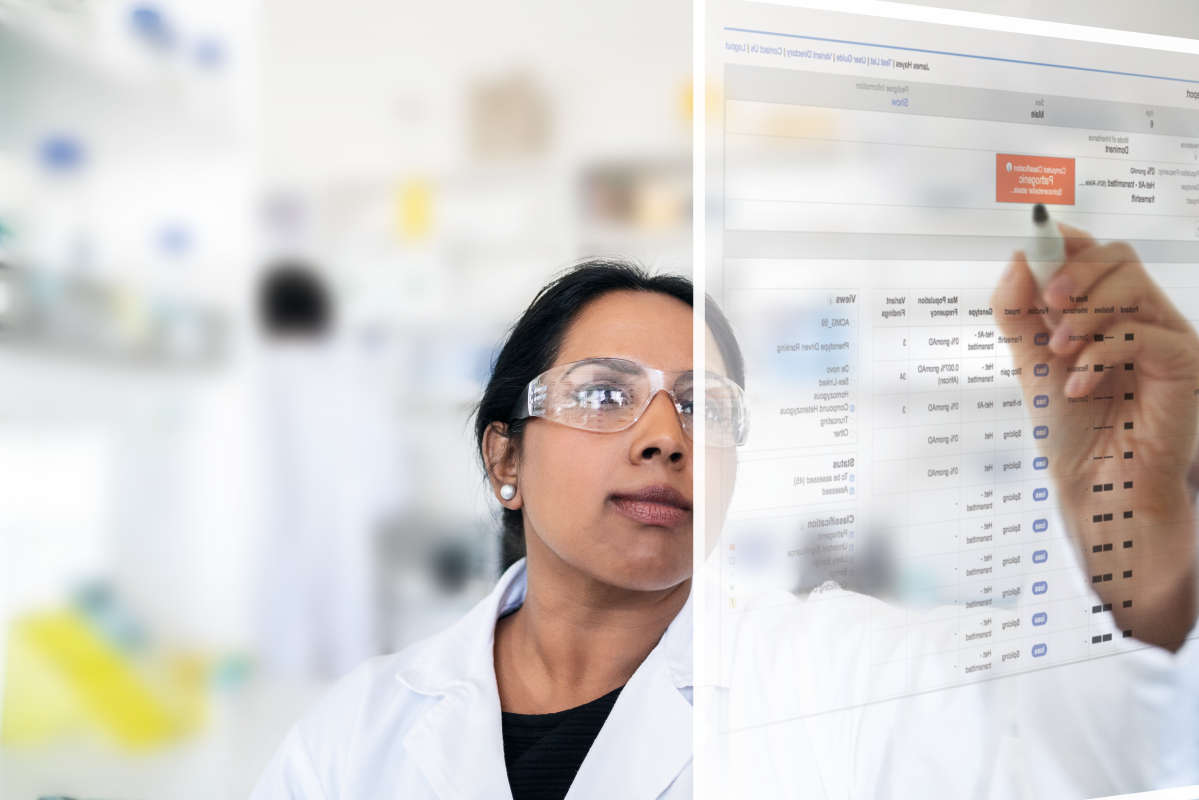
Scientists around the world are racing to learn more about the ongoing Ebola virus outbreak in West Africa, which as of November 2014 had claimed nearly 5,000 lives and infected more than 13,000. Thanks to remarkable new work from researchers at the University of Washington and collaborators at the University of North Carolina and Rocky Mountain Laboratories, there’s a new tool in the battle against this virus: a collection of mouse strains that closely models the types and progression of Ebola seen in humans. Until now, scientists seeking to understand virus biology or screening drug compounds, among other activities, were limited in their ability to use model organisms. The mouse model for Ebola did not display similar phenotypes to humans infected with the virus. Conducting research on the organism that best models human response to Ebola — the primate rhesus macaque — is expensive, challenging, and ethically complicated, says Angela Rasmussen, a research assistant professor in the microbiology department at the University of Washington and lead author on this new project. Rasmussen and her colleagues aimed to design a better model, and they started with a community resource that has successfully delivered improved mouse models for other research areas: the Collaborative Cross program at the University of North Carolina. She also pulled in another tool that has worked well for her in the past: Ingenuity Pathway Analysis (IPA) from QIAGEN, which she deploys to analyze complex transcriptomic data. For other parts of the data analysis workflow, CLC Genomics Workbench was used for assembly and variant detection on sequencing data. Between these tools, Rasmussen not only developed an important new model for Ebola research, but she also discovered significant details about effects of host genetics on infection outcomes. Her team’s findings are reported in an October 2014 publication in Science entitled “Host genetic diversity enables Ebola hemorrhagic fever pathogenesis and resistance.” Virus Hunter With a background in microbiology, Rasmussen now specializes in RNA viruses and other emerging viruses. “My overall interest is applying systems-level techniques — transcriptomics, proteomics, metabolomics — to understand the host response to virus infection and how that leads to a pathogenic outcome, or potentially how that can be exploited for therapeutic purposes,” she says. In the past few years she has worked with a host of viruses, including influenza, hepatitis C, rhinovirus, and Ebola. While Ebola is front and center on the global stage today, Rasmussen says, it’s typically a fairly neglected member of the emerging virus community. She began her quest for a better mouse model three years ago, when there was no pandemic shining a spotlight on the virus. At the time, the existing mouse model for Ebola “left a lot to be desired,” Rasmussen says. The virus would kill the mice, but wouldn’t cause hemorrhagic fever, a common component in human infections. “You couldn’t study the full range of Ebola virus phenotypes with that model,” she notes. Realizing this limitation, Rasmussen knew just where to start: the Collaborative Cross program, a dedicated effort to generate more genetically diverse mice that would better mirror the diversity of human phenotypes for any number of disease studies. The project hinges on a complex eight-way funnel breeding system that mixes five classical lab strains with three wild-derived strains. The resulting mice are genetically distinct from one another and represent about 90 percent of potential diversity across the entire mouse species, while still having very well-characterized genomes suitable for in-depth genomic studies. “We had already seen expanded phenotypic ranges when we infect the Collaborative Cross mice with influenza,” Rasmussen says. “We decided to take Ebola virus and infect these mice. Just as with influenza, we saw an expanded phenotypic outcome.” The new mice, featured in the paper published in Science, display all three major phenotypes seen among humans infected with Ebola: hemorrhagic fever, death, and resistance to lethal infection. “We can now use mice to really model the full breadth of Ebola outcomes that we see in human populations — for example, in the current outbreak,” Rasmussen says. She and her team hurried to make this advance public to help scientists battling the current Ebola outbreak. Their new mouse model is available through Collaborative Cross at the University of North Carolina and can be used with Ebola virus by any scientist from a BSL4 containment facility. “We wanted to publish this to make it available to other researchers so they know this is an option for screening drug candidates and vaccines,” Rasmussen says. “If you have five different candidate drugs, this could help you narrow it down to the most promising one.” Host Genetics Rasmussen’s paper details the comprehensive characterization work the team performed to validate the genetics of the new mouse model and its accurate representation of human response. In the process, they uncovered promising clues about why some targets of the Ebola infection show resistance while others get hemorrhagic fever and die. In the publication, the authors describe an analysis of two lines of the mice, one that died from hemorrhagic fever and another that was resistant to infection. They collected longitudinal samples from liver and spleen, the organs most targeted by Ebola virus. Rasmussen then examined transcriptomic data generated from those samples and performed differential gene expression analysis. She loaded that information into IPA and looked for biological elements “that might mechanistically explain why some animals were developing hemorrhagic fever while others were not,” she says. That resulted in an “aha!” moment for Rasmussen, who found that the liver samples from hemorrhagic fever-susceptible animals had two strongly downregulated tyrosine kinases, TIE1 and TEK. Liver is typically where coagulation factors are produced. Further analysis with IPA revealed that these tyrosine kinases “were associated with a bunch of genes that have been speculated to be involved in hemorrhagic fever pathogenesis,” Rasmussen says, “so I used the Molecule Activity Predictor function in IPA to model the effect that that would have on some of those genes of interest as well as some of the genes that came up in my data set.” Indeed, results indicated a profound effect on increases in coagulation factors, which has been speculated to be a response related to the onset of hemorrhagic fever symptoms. “The biology of it made a lot of sense to me,” Rasmussen says. But Rasmussen is still pursuing the Ebola work. “We’re considering this a relatively preliminary finding. Our plan ultimately is to do transcriptomics on a lot of these mouse lines and try to narrow down genes that are common to one phenotypic outcome or another and essentially use them as biomarkers,” she says. At this point, the team has screened nearly 50 lines of the Collaborative Cross mice, finding symmetry between phenotype segregation in mice and the current outbreak of Ebola in Africa. “It’s an ongoing screen,” Rasmussen says. “The next step is to really take advantage of the genetic resources associated with the Collaborative Cross and start linking genetic loci to phenotypic outcome.” For her own work, she’ll be focusing on transcriptomic studies of those liver and spleen samples the team has continued to collect. “We’re running microarrays on them right now, and of course I’ll use IPA to do the functional analysis on those,” she says. Digging in the Data Rasmussen first came across IPA several years ago, when she used it for a hepatitis C virus (HCV) project during her postdoctoral fellowship. She was taking advantage of a unique opportunity to study full HCV progression from the moment of infection by following liver transplant patients who acquired the virus along with their new organ. What she wanted to know was: why did some transplant patients progress to severe liver disease more quickly than others? “We had longitudinal biopsies collected from these liver transplant patients,” Rasmussen says. After generating transcriptomic data and using mathematical analysis to identify outcome-predictive genes, she dug in with IPA to determine the function of those genes. Since then, improvements and feature additions to IPA have made the platform even more valuable for her studies. Rasmussen finds the functional categories, heat map layout, and Upstream Regulator Analysis particularly useful in her work, where biological results from viral infections don’t always fit neatly into canonical pathways. As the virus manipulates the host response, she has found it necessary to start with relevant functional categories and then drill down, developing her own networks and customizing her analysis based on the experimental system — all of which is possible with IPA. She also appreciates the links back to papers so she can easily review the supporting literature for results presented. “When you’re doing transcriptomics or systems biology, IPA is really an indispensable tool,” Rasmussen says.
Download full text PDF of this study Learn more about CLC Genomics Workbench Learn more about Ingenuity Pathway Analysis (IPA)