
















Treatment options for ovarian cancer haven’t changed much in three decades — but a powerful new biomarker identified by scientists at Mount Sinai has shed light on why some patients respond well to the gold-standard chemotherapy regimen while others do not. They discovered IRF1 in just seven samples with Ingenuity Pathway Analysis from QIAGEN.
Seven years ago, two scientists hatched a plan for an oncology resource that would be far better than what was available to them at the time. Today, that resource has paid off in ways even its founders couldn’t have predicted.
John Martignetti, an Associate Professor at the Icahn School of Medicine at Mount Sinai, teamed up with his colleague and Director of Gynecologic Oncology Peter Dottino seven years ago to launch a program on ovarian cancer. That collaboration led to the creation of a biorepository with data and tissue samples for gynecologic oncology patients who choose to participate. Factors that make this biobank unique are its longitudinal collection of blood and tissue specimens, creation of cell lines for all tumors, and the development of animal models for some patients as part of the personalized cancer therapy program at the Icahn Institute for Genomics and Multiscale Biology.
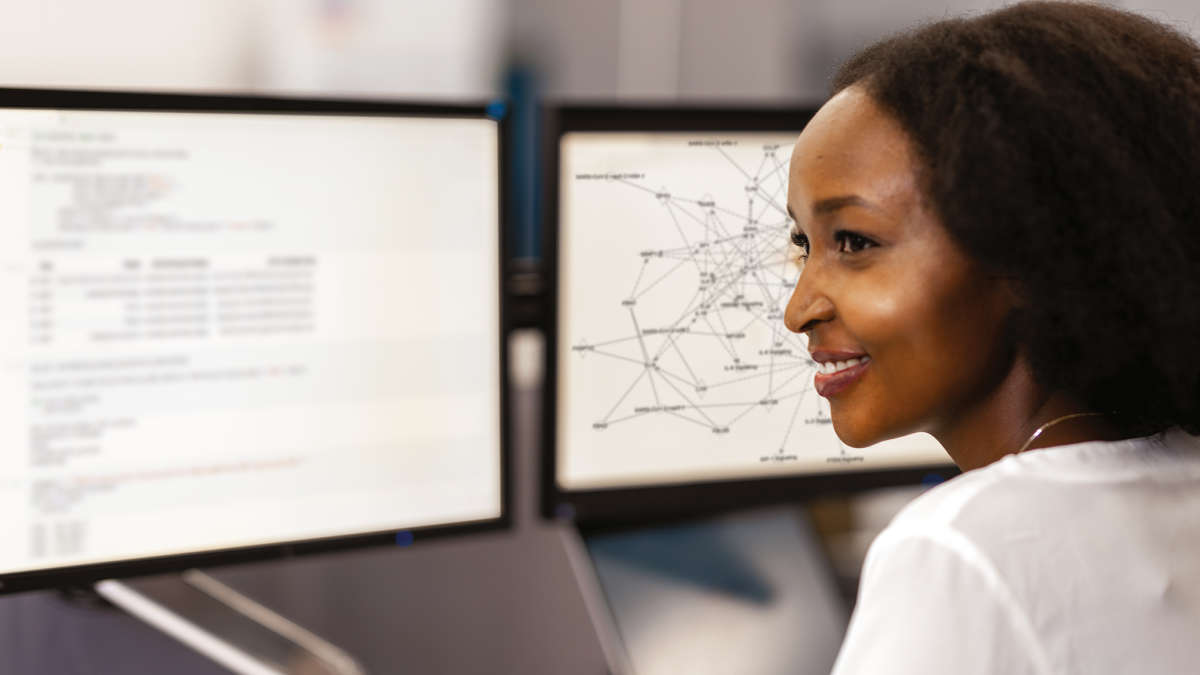
Today, this remarkable resource is the foundation for a number of innovative studies in ovarian cancer, including new work from Martignetti and his lab that identified a novel prognostic biomarker indicating whether a patient will respond well or poorly to the standard chemotherapy used for this aggressive type of cancer. The biomarker, which had not previously been linked to ovarian cancer, was found with QIAGEN’s Ingenuity Pathway Analysis (IPA), a leading application for interpreting biological data and modeling complex networks. Now scientists are studying how the biomarker, interferon regulatory factor 1 (IRF1), functions and whether upregulating it might improve ovarian cancer patients’ outcome in the future.
As Martignetti and Dottino envisioned it years ago, the Mount Sinai ovarian cancer resource would not only include relevant tissue — lots of biobanks did that — but it would also link to patient data from test results to follow-up visits and more. Participation is voluntary; once patients opt in, they are included in the repository from their very first surgery at Mount Sinai. “It starts from the day of contact prior to their next meeting in the operating room,” Martignetti says. “Patient information is entered into a HIPAA- and IRB-compliant database where records are linked to the samples that we collect at the time of surgery and throughout their care over many years.”
That spectrum of information on each patient is one feature that makes this biobank more powerful than other repositories. “We’ve tried to be very careful about linking all the patient data in real-time,” Martignetti says. “That initial tumor source is not just a static piece of information; it’s continuously updated.”
Samples can include fresh frozen tumor from the surgery as well as fluid and blood samples taken in follow-up sessions. Tumor samples also go to the lab, where researchers start cell lines for each patient’s cancer. They extract DNA, RNA, and protein and store them for future studies. Building these cell lines for each patient “has been a long, arduous task, but we remain confident it is critical,” Martignetti says. “Now if we’re interested in looking at a potential new therapeutic or doing a biochemical or genetic study, we’ve actually got cell lines from these patients.”
An unexpected advantage of the biorepository stems from how closely its gynecologic oncology team works together. The process for treating the many ovarian cancer patients who come through Mount Sinai’s doors is so standardized that it minimizes variability in surgical technique and follow-up care. This consistency means that differences seen among the biobank samples likely represent real genetic variation rather than external influences, Martignetti notes.
Recently, the team behind the biobank has added animal modeling to its repertoire. Through the personalized cancer therapy effort at the Icahn Institute, scientists implant tumor cells from patients into mice, and then use those models to test the effects of different therapeutics.
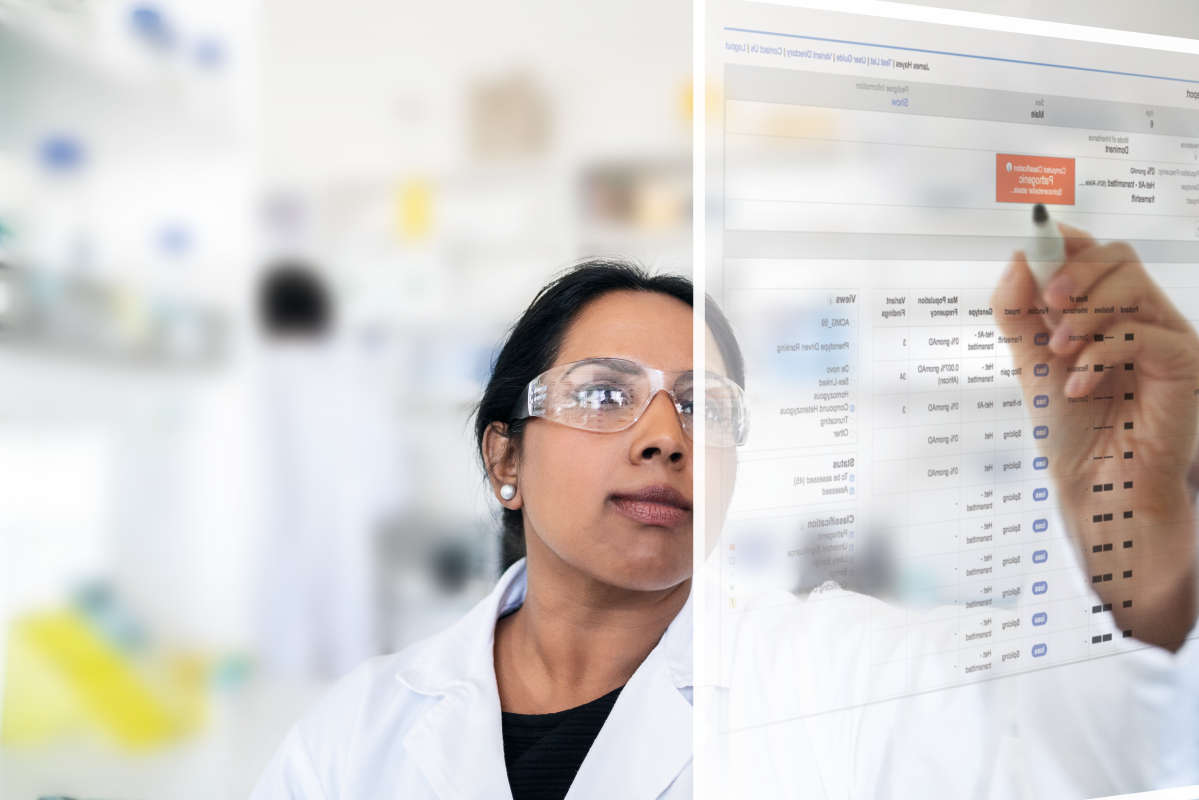
In a project detailed in a recent publication in the journal Gynecologic Oncology, Martignetti and his colleagues used their biorepository to answer a question that challenges clinicians everywhere: Why do some patients respond well to chemo while others become resistant?
“The first therapeutic treatment for every ovarian cancer patient, no matter where you are in the world, is a combination of a platinum agent and taxol,” Martignetti says. “That’s been the standard for 30 years now.” Patients who experience a recurrence of the disease during the first year of cisplatin treatment are classified as platinum-resistant; patients who don’t are considered platinum-sensitive. “Because that status is important to understanding patients’ long-term outcome as well as how they’ll be treated in the future, we were very interested to know if there was something that would have predicted their response to a platinum agent at the original time of surgery,” he adds.
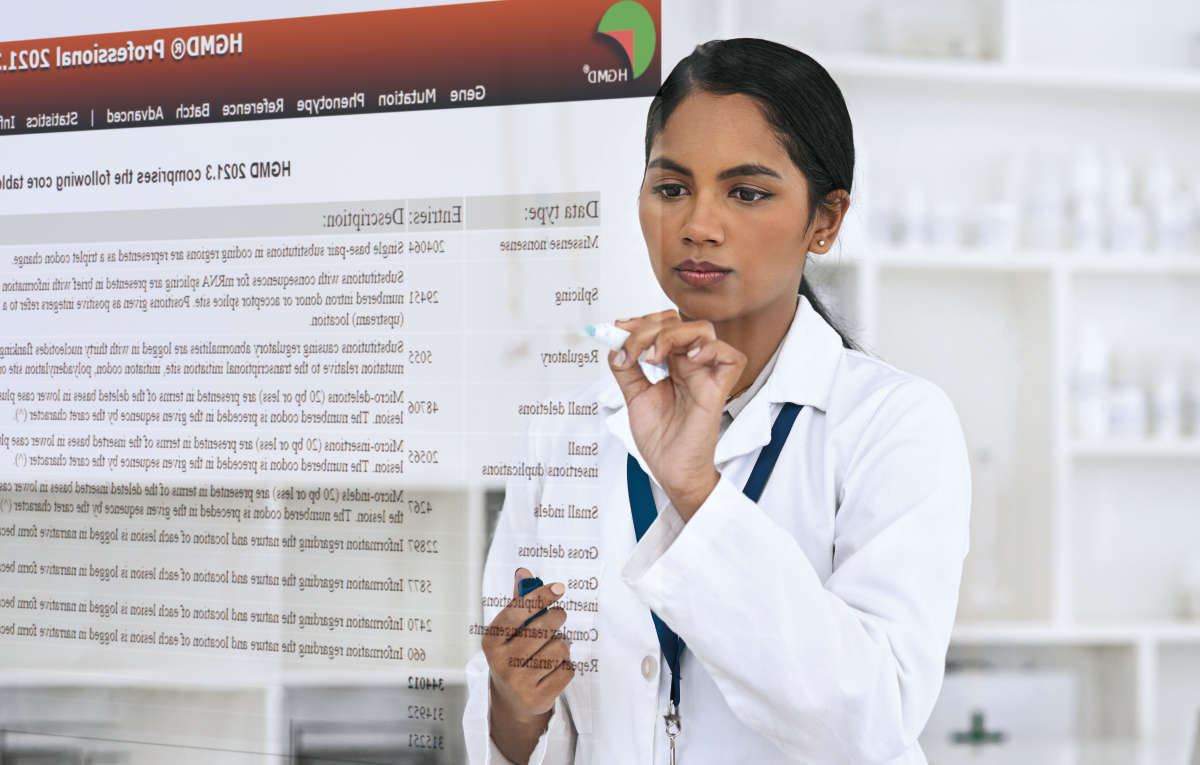
So they dug into their biorepository, choosing just a few samples: four from people who eventually became resistant to platinum treatment, and three from patients who remained sensitive to the treatment over time. Martignetti’s team performed a complete transcriptome analysis of the samples to determine whether gene expression levels in the tumors would have revealed each patient’s outcome.
“That’s when we turned to IPA,” he says. Martignetti collaborated with QIAGEN scientists Jean-Noel Billaud and Richard Halpert for intensive analysis of the transcriptome data. “Using IPA and the Upstream Regulator Analysis module, with just seven cases, we found two really strong predictors for differences between the platinum-sensitive and the platinum-resistant patients,” he says. These two biomarker candidates, IRF1 and IRF7, were both linked to immune response — and conveniently, the former activated the latter, so the scientists focused their studies on IRF1.
Martignetti is still impressed that IPA was able to find the IRF1 signal in such a small sample set. “That speaks to the power of the analysis system and to the power of having really well annotated and curated samples,” he says.
Of course, identifying IRF1 from so few samples made it a candidate — but one that needed to be validated. “Next we went to a group of 31 samples and looked at the expression levels of IRF1 and its association to platinum sensitivity,” Martignetti says. “It held up perfectly.”
Finally, the team went beyond their biorepository to an online tool called KM plotter, which incorporates data from The Cancer Genome Atlas initiative as well as the Gene Expression Omnibus. Looking at IRF1 expression levels across more than 1,200 high-grade serous ovarian cancer samples, the data matched up again. “If you have high IRF1 levels, you have better progression-free survival and better overall survival rates,” Martignetti says.
Having that information ahead of time could help inform the clinician about whether to consider treating patients differently — for example, being more aggressive with patients who are more likely to become resistant. Alternatively, patients with a poor prognosis would have more information to use in their decision on whether to move forward with treatment, since quality of life is an important element to consider.
Martignetti says that IPA was an instrumental analysis tool in this project. “The Upstream Regulator Analysis was important in pulling together all the disparate pathways that were being activated and upregulated to find the commonality of the IRF1 pathway,” he says. “That’s not something we could have done manually. We would not have seen that relationship without IPA.”
The tool also allowed Martignetti to play a larger role in the data analysis. “With IPA, a non-bioinformatician like myself can use the web interface and take part. I can understand the parameters and be involved in the selection criteria of the genes, for example,” he says.
With this project published, Martignetti and his team already have plans to delve more deeply into IRF1 and the ultimate possibility of regulating it to help patients. “Having identified the pathway doesn’t mean we understand why it’s making a difference,” he notes. “Once we understand it, can we somehow modulate it? Would making IRF1 levels higher improve survival benefit?” The group also plans to follow up on other pathways highlighted by IPA, analyze additional variables, and find even larger data sets to interrogate. Ultimately, the Sinai team’s goal is simple: they want to generate findings that “have relevance to the clinician and to the patient,” Martignetti says.