














Centers for Disease Control and Prevention (CDC) released on November 13, 2019 their report Antibiotic Resistance Threats in the United States, 2019, showing that antibiotic-resistant bacteria and fungi cause more than 2.8 million infections and 35,000 deaths in the United States each year. This is striking, indicating that on average, someone in the US gets an antibiotic-resistant infection every 11 seconds, and that every 15 minutes someone dies from one. Check out the coverage on Twitter by following #CDCARThreats.
Nevertheless, data from the new report show progress in fighting these infections. Since 2013, prevention efforts have reduced deaths from antibiotic-resistant infections by 18% overall and by nearly 30% in hospitals. Rapid detection and prevention strategies in communities have helped protect people from two community-associated germs: vaccines have helped reduce infections from Streptococcus pneumoniae in many at-risk groups, and the cases of drug-resistant tuberculosis (TB) in the United States remain stable due to effective TB control strategies.
However, CDC is concerned about antibiotic-resistant infections that are on the rise including:
This new data show that continued vigilance is needed to maintain the progress seen thus far. Further preventing infections and stopping the spread of germs will save more lives.
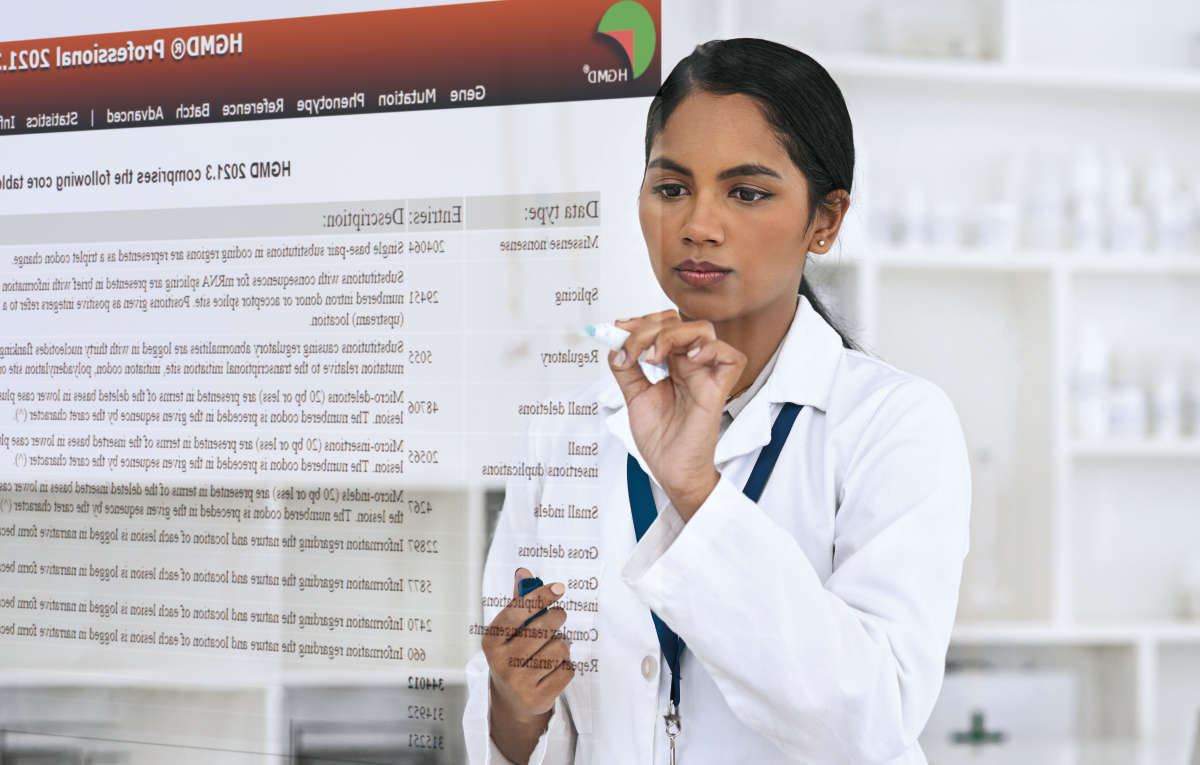
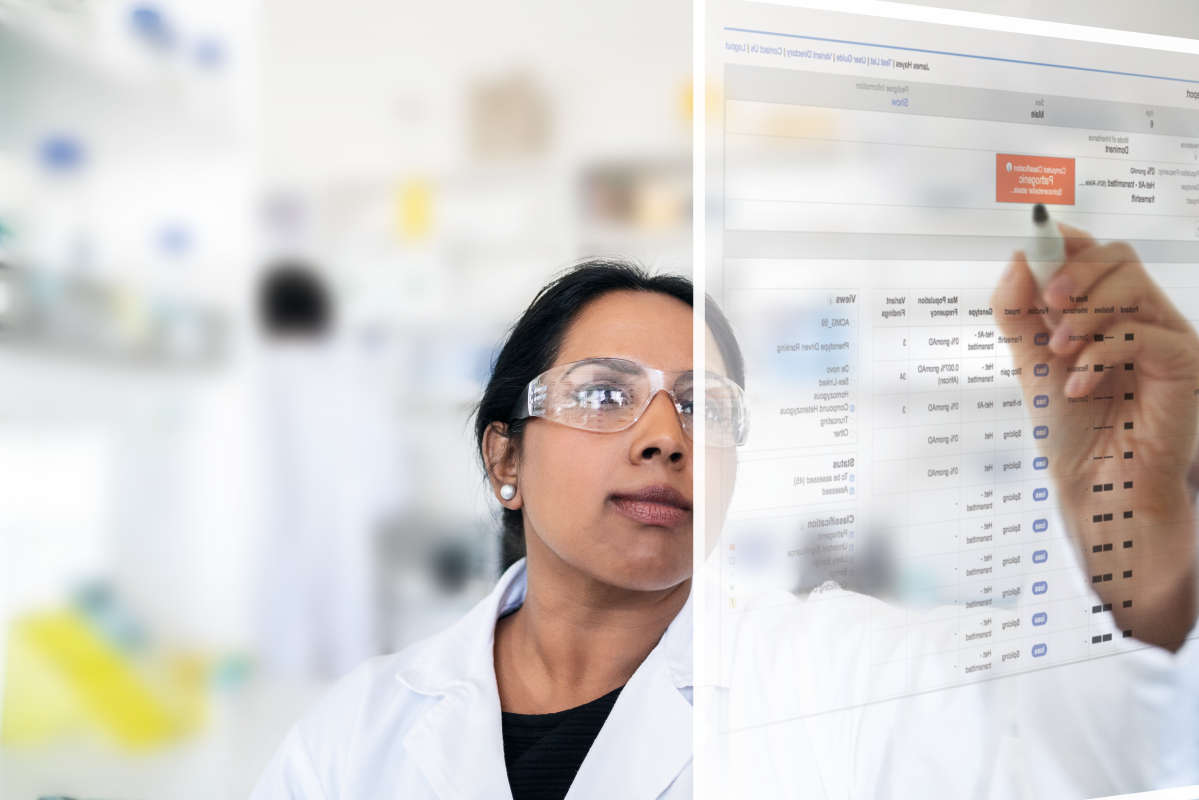
QIAGEN offers tools and solutions to support public health epidemiology, clinical microbiology research and basic microbial genomics research. QIAGEN CLC Microbial Genomics Module offers unique and valuable features and functionalities to help advance research of microbial infections and their prevention. These capabilities include:
Learn more about the QIAGEN CLC Microbial Genomics Module and check out the details of how this tool can support you in the fight against emerging antimicrobial resistant (AMR) pathogens.
QIAGEN is committed to supporting advanced research into the underlying drivers of antimicrobial resistance. Earlier in 2019, as a statement of our commitment, we were the first bioinformatics company to join the joint United Nations - CDC Global AMR Challenge. Read more about our commitment and the new QMI-AR database here.
References:
CDC (2019). Antibiotic Resistance Threats in the United States, 2019. Atlanta, GA: U.S. Department of Health and Human Services, CDC.