















But the upshot of the study was sobering for those who believe that genome sequencing is speeding to the clinic: there were far more disease-causing mutations discovered than people who actually had any disease. Of the 11 people who got reports saying their genomes harbored variants that should cause disease, only two of them actually had the disease. These conditions are not ones expected to have unusually late onset.
From our perspective, these results are not an indication that genomics has little to contribute to healthcare; instead, they are a stark reminder that efforts to accurately interpret the genome still have a long way to go. Programs like the Allele Frequency Community should help with this, but what we need most of all are more genome sequences and really strong phenotype/clinical data associated with them so that we can hone interpretation algorithms.
For the nine people who were expected to have a disease based on their genomic data but didn’t, it is likely that we will eventually discover protective mechanisms that offset the mutation, or perhaps environmental or dietary factors that explain the disconnect. For now, though, we are still at the earliest stages of truly understanding the human genome, and that’s the main message of the MedSeq results.
At QIAGEN Bioinformatics, we’re working hard to make sure that our genome analysis and interpretation tools incorporate the newest discoveries, rely on high-confidence findings, and help scientists see the big picture of how various mutations, pathways, and other factors fit together. We applaud the MedSeq team for drawing attention to this important topic.
It is not surprising to find mutations that are disease causing in healthy people because almost none of the known disease-causing mutations are 100% penetrant, or predictive of developing the resulting disease in all cases. If you get the disease depends on genomic context – some diseases are late onset and depend on your age, while others can manifest in a spectrum of how strong the effect is, and the effect may be below the threshold of calling it out as a disease.
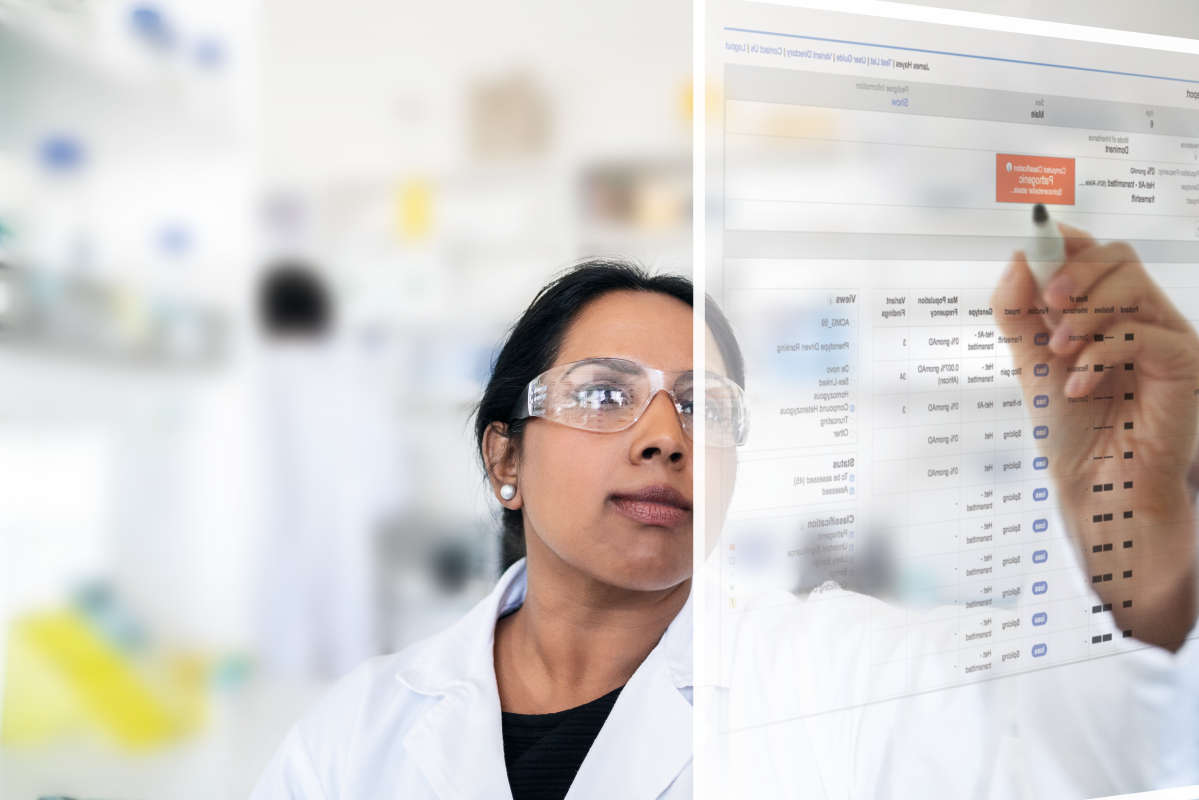
That's why our software solutions allow for phenotype supported ranking: the ability to combine observed phenotypes of the patients with the genomic data for better interpretation results. Because of the insights we have in our QIAGEN Knowledge Base about mutations, genes, diseases, phenotypes and their relationships, we are able to prioritize mutations that are related to the individual phenotype, and we can show that this increases the rate of resolving causative mutations.